Published at Journal Asian Hospital & Healthcare Management
issue 63 , February 2024
Transforming Pressure Injury Detection
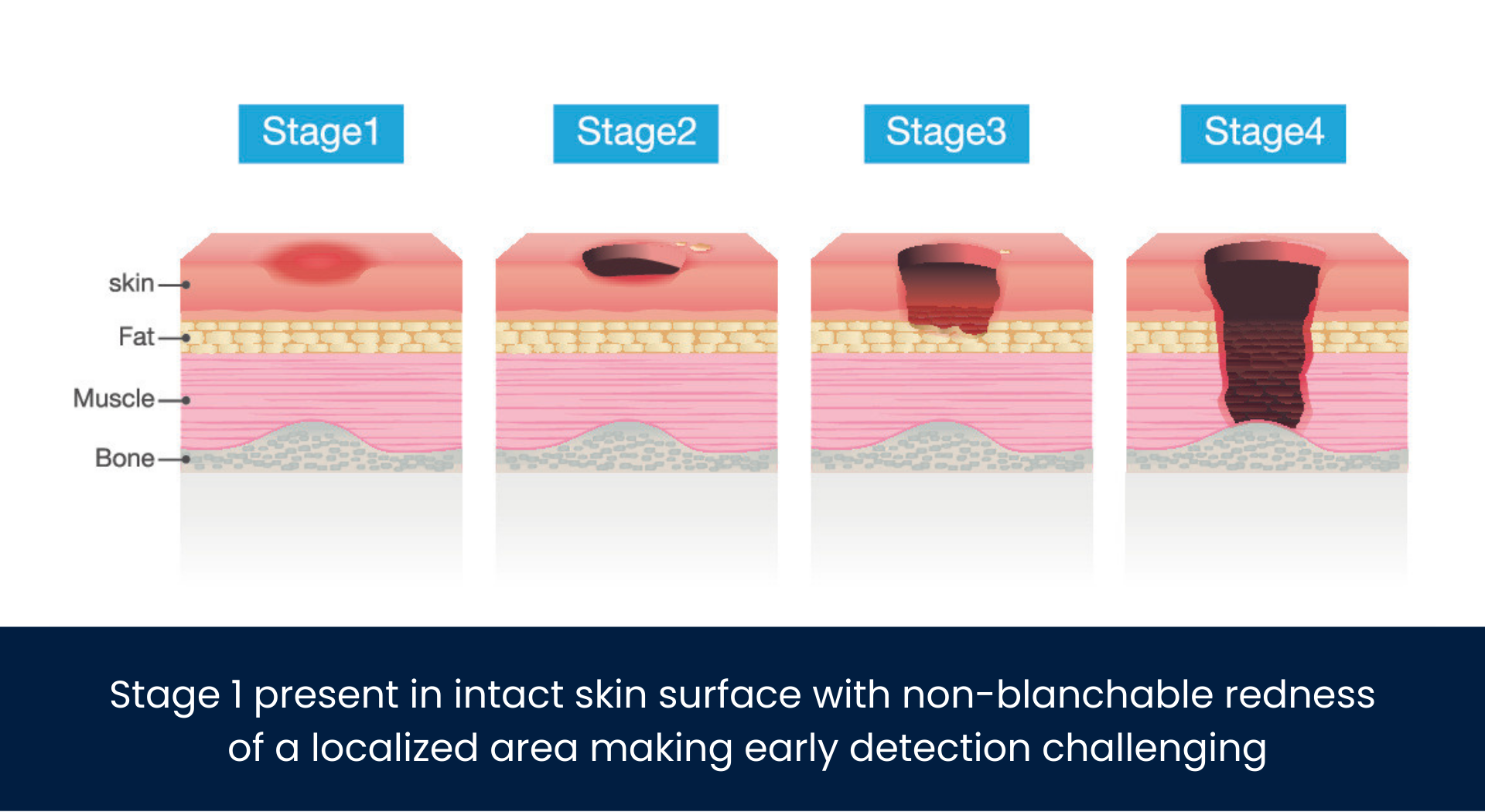
Pressure injuries are a global healthcare concern leading to significant suffering and healthcare costs. Recent advancements in biotechnology and AI have emerged as promising tools in early pressure injury detection and prevention. AI, combined with non-invasive Infra Red subepidermal biomarker detection, can enhance healthcare practices for pressure injuries, leading to improved outcomes.
Pressure injuries are a persistent healthcare challenge worldwide, causing immense suffering to affected individuals and imposing substantial economic burdens on healthcare systems. These wounds result from prolonged pressure on the skin, frequently affecting immobile or bedridden patients. Most pressure injuries occur over bony prominences, such as heels and sacrum, where there is compressed or diminished tissue. Early detection and timely intervention are critical in mitigating the impact of pressure injuries.
Currently, visual inspection is used to detect and classify pressure injuries according to depth, width, degree of tissue loss and presence of granulated tissue. However, these traditional detection methods can suffer from subjectivity and error. In recent years, biotechnology and AI have emerged as potential game-changers in the realm of pressure injury management.
The transformative potential of AI, along with sub-epidermal biomarker detection, can improve healthcare practices for pressure injuries, with a focus on enhancing patient outcomes, improving equitable treatment, and reducing healthcare costs.
The Global Burden of Pressure Injuries
Pressure injuries are a global healthcare concern with a substantial incidence rate. According to a meta-analysis published in the International Journal of Nursing Studies, one in ten adults admitted to hospitals are affected. Another article published in BMJ Open Quality states hospital-acquired pressure injury incidence ranges from between 18.1% to 26%. In the U.S. alone, where 2.5 million people develop pressure injuries each year, 60,000 people die as a direct result of these injuries according to data from the National Pressure Injury Advisory Panel. Life threatening conditions resulting from pressure injuries include:
- Infections: Pressure injuries can become infected, leading to complications such as cellulitis, an infection of the skin and connected soft tissues, and sepsis, a potentially life-threatening infection of the blood. Pressure sores can also burrow into joints and bones, causing bone and joint infections that impact the function of the joints.
- Cancer: Long-term wounds that don’t heal can lead to squamous cell carcinoma.
- Damage to Muscle, Bone, or Joints: The damage from pressure injuries can extend to the muscle, bone, or joints. This can lead to a serious infection of the bone, known as osteomyelitis.
Moreover, hospital acquired pressure injury rates are increasing while all other hospital acquired conditions are decreasing. In fact, pressure injuries occur across the healthcare spectrum in the U.S.: 10% of patients in acute care get pressure injuries; 25% of patients in long term acute care; 12% of patients in nursing homes; and 12% of patients in rehabilitation centers, according to the National Pressure Injury Advisory Panel. These injuries are not only physically painful but also carry a significant economic burden.
The Cost of Pressure Injuries
Pressure injuries exact a substantial financial toll on healthcare systems worldwide. The cost of treating pressure injuries includes hospital stays, wound care supplies, medications, and surgical interventions when wounds become severe. According to data from the National Pressure Injury Advisory Panel, the annual cost of pressure injuries in the United States alone was $26.8 billion in 2019. Patient care cost per pressure injury ranges from $20,900 up to $151,700 in the U.S. It is one of the five most common harms experienced by patients and the second most common claim for lawsuits after wrongful death.
Major Healthcare Inequity Issue
Due to the current standard of care method of visual inspection of the skin, pressure injuries can be harder to detect in people who have darker skin. While this is certainly a global challenge, the disparity is perhaps most evident in the U.S. which has one of the most diverse populations on the planet. According to a study published in Wounds, Research shows that people with dark skin tones in the U.S. suffer from pressure injury more than twice as much as those with lighter skin. They have higher pressure injury rates, higher risks of mortality from pressure injuries, and more severe pressure injuries. While white patients had the lowest incidence of pressure injuries, among all racial and ethnic groups in the U.S., black patients had the highest. Underscoring the need for improved skin assessment techniques for people with dark skin tones, a study in Advances in Skin & Wound Care states the diversity index in the U.S. has increased to 61.1% in 2020 and worldwide, people with dark skin tones comprise a majority of the population.
A skin-color agnostic technology that can detect pressure injuries beneath the skin’s surface, which is less influenced by the melanin content, could significantly address these challenges.

AI and Subepidermal Biomarker Detection & Analysis: A Promising Approach
AI is accelerating the pace of research, with its primary contribution being to serve as a decision support system for identification of specific disease states and their corresponding treatments. The enhanced capabilities in disease testing and the determination of their causes through biomarkers have opened up new avenues for more precise diagnoses. This includes the creation of noninvasive early-stage detection tools that can influence specialist decision-making, streamline medical treatments, and reduce healthcare costs.
Furthermore, AI-driven diagnostic tools delve deep into biomaterial analysis, reaching down to the cellular level. They not only examine individual cell components but also process entire cell samples to pinpoint deficiencies and identify the most suitable treatments. This personalized approach to treatment has become a reality thanks to AI, marking an exciting development in the field of medicine.
By providing objective and precise assessments of subepidermal biomarkers, AI can significantly reduce the risk of human error and improve the accuracy of early detection across numerous diseases and conditions. AI plays a central role in not only in sending but also in analyzing data from subepidermal biomarkers. The adaptability of AI to changing patient conditions enhances its predictive capabilities.
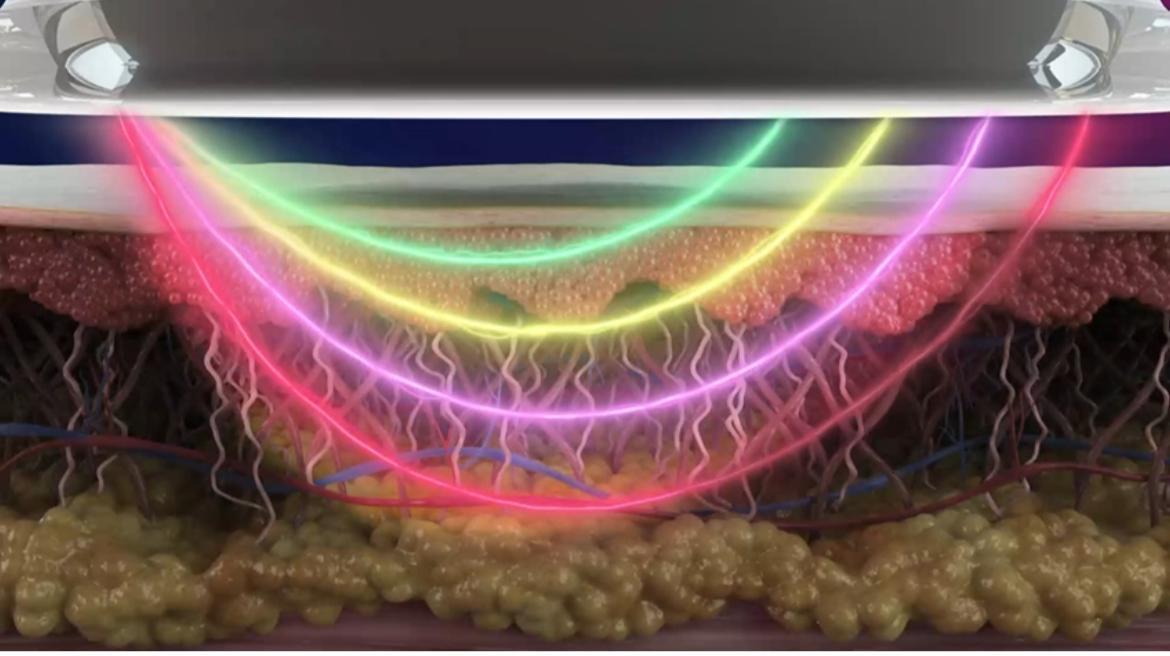
Figure 1 Infrared light harmlessly penetrates deep below the patient’s skin in less than a second. The pattern and intensity of light is captured by miniature sensors.
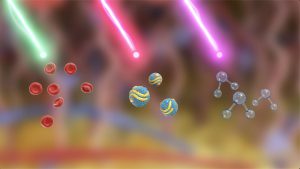
Figure 2 The light captured by the sensors capture bio info from targeted markers in blood and tissue.
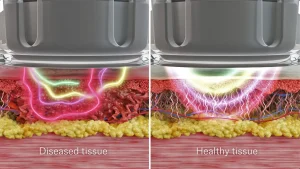
Figure 3 Healthy and diseased tissue absorb and reflect light differently, allowing biomarker profiling.
Pressure injuries are a prime example of how AI can produce benefits in healthcare. Subepidermal biomarkers offer a promising avenue for early pressure injury detection. These biomarkers, located beneath the skin’s surface, can signal tissue damage before visible symptoms appear. Emerging research in this field demonstrates the feasibility of detecting subepidermal biomarkers, thereby enabling timely interventions to prevent bedsores.
One model for how this might work is the use of a handheld device that contains miniaturized electro-optics emitters and passive sensors that send and detect visible light and infrared light. The light can be used to acquire biological information by assessing light reflected from different layers under the skin’s surface down to the reticular dermis. Optical properties of biological tissue change the spectrum of reflected or absorbed light in accordance with the tissue’s structural and chemical composition including chromophore content such as water, collagen, oxyhemoglobin and melanin. Blood flow can be measured, as blood flow in pressure injuries is different from that in healthy tissues based on measures of blood cell perfusion in the microvasculature. Sensor results can then be classified and analyzed by an AI cloud-based system at the point of care into the predefined conditions.
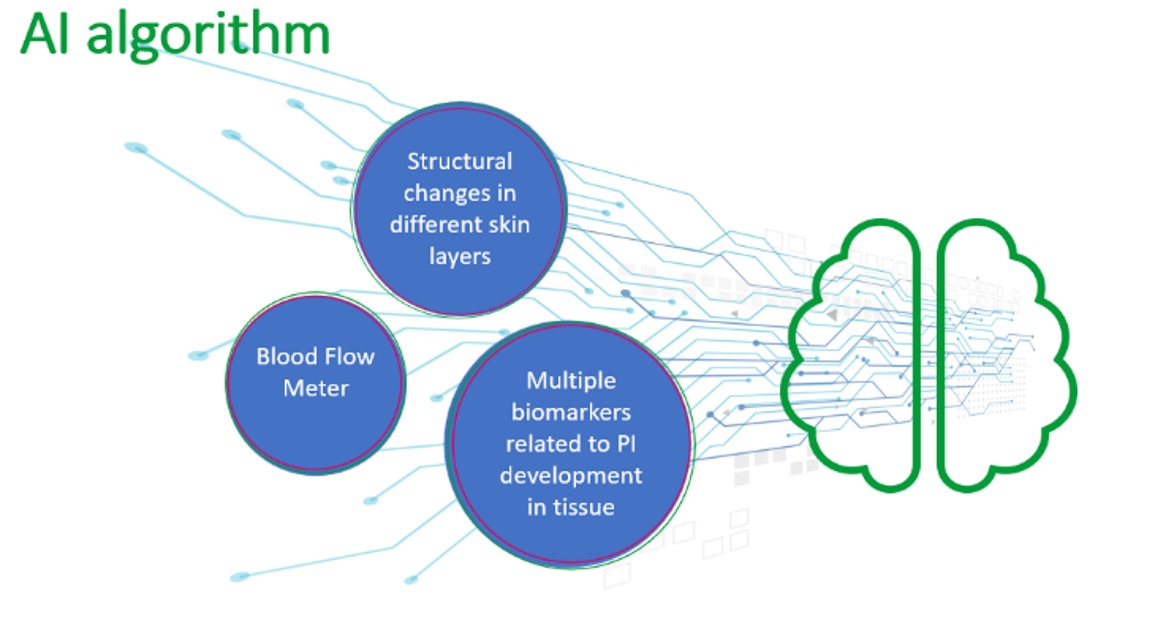
Using this kind of model, AI algorithms can swiftly identify pressure injury risk factors, enabling healthcare providers to formulate personalized prevention plans tailored to individual patient needs. The algorithm itself can be driven by data from the three primary sources analyzed: 1) multiple
biomarkers related to pressure injury development in tissue; 2) structural changes in different skin layers; and 3) blood flow meter.
Transformative Implications for Healthcare
The integration of AI and subepidermal biomarker detection into pressure injury management holds immense transformative potential for healthcare including:
- Enhanced Patient Outcomes: AI-driven early detection can significantly improve patient outcomes by enabling timely interventions. The reduction in the severity and incidence of pressure injuries can lead to better quality of life for affected individuals and even save lives.
- Reduced Healthcare Costs: The adoption of AI in pressure injury prevention can lead to substantial cost savings for healthcare systems globally. By averting the need for costly treatments and interventions, healthcare expenditures can be minimized.
- Objective Assessments: AI offers standardized and objective assessments, irrespective of geographical location. This ensures consistent quality of care and minimizes regional disparities in pressure injury management.
Challenges and Future Directions
While the potential of AI and subepidermal biomarker detection in pressure injury prevention is promising, challenges must be addressed for widespread implementation:
- Integration into Electronic Medical Records and Data Standardization: Capturing and analyzing biomarker data using AI is a tremendous asset that needs to be integrated into patient and hospital electronic medical records. This calls for the need for data standardization and when needed, data sharing among various healthcare providers.
- Education and Training: Ensuring that healthcare professionals worldwide receive training in AI utilization for pressure injury prevention is crucial for realizing the technology’s full potential.
- Ethical and Health Equity Considerations: Ethical considerations surrounding AI in healthcare must be addressed universally to ensure responsible and compassionate use of these technologies. In the case of pressure injuries, AI can help improve ethics in healthcare through the combination of seeing beneath the skin’s surface and being a skin-color agnostic technology, thereby addressing inequities based on race and skin color. It is important that such a technology be universally adopted across various socio-economic groups and geographic regions.
Conclusion
Pressure injuries represent a significant healthcare challenge, causing suffering to patients and straining healthcare budgets globally. The integration of biotechnology and AI, along with subepidermal biomarker detection, holds immense promise in addressing these challenges and revolutionizing pressure injury prevention. As healthcare envisions a future empowered by AI, the focus on improving patient outcomes and reducing healthcare costs through AI-driven approaches is pivotal. The synergy of AI and subepidermal biomarker detection offers a beacon of hope for patients and healthcare systems worldwide, ultimately leading to enhanced patient well-being and more efficient healthcare practices.
Author Biography
Yaniv Cohen, PhD MSc, Co-Founder & Chief Science Officer of IR-MED is a skilled scientist and entrepreneur with years of experience leading R&D development for medical device companies. His fields of expertise include electro-optics, infrared spectroscopy, AI, and medical devices using infrared light. PressureSafe™, co-invented by Dr. Cohen, is an early detection device for pressure injuries.